Are Your Teeth Destroying Your Joints?
The Invisible Inflammation Fueling Rheumatoid Arthritis & Osteoarthritis
The Impact of Oral Health on Bone Health: Insights into Rheumatoid and Osteoarthritis
Emerging research continues to reveal complex interactions between oral health and systemic conditions, including bone-related diseases such as rheumatoid arthritis (RA) and osteoarthritis (OA).
While RA and OA differ significantly in pathophysiology, both conditions demonstrate potential associations with the oral microbiome. Understanding these relationships may improve early detection strategies and therapeutic outcomes.
Rheumatoid Arthritis and Oral Health
The Role of Periodontal Pathogens
Rheumatoid arthritis is a chronic, systemic autoimmune disease characterized by joint inflammation and destruction. Numerous clinical studies have identified a strong correlation between RA and periodontal disease.
A key player in this association is Porphyromonas gingivalis, a periodontopathic bacterium implicated in RA pathogenesis through its ability to induce protein citrullination. Protein citrullination is like your body accidentally editing its own instruction manual.
Normally harmless, this tiny chemical change (converting arginine to citrulline in proteins) can confuse your immune system into attacking your own tissues, triggering diseases like rheumatoid arthritis, especially when gum disease bacteria hijack the process. This modification leads to the formation of anti-citrullinated protein antibodies (ACPAs), a hallmark of RA.
Moreover, P. gingivalis infection elevates pro-inflammatory cytokines such as TNF-α, IL-1, IL-6, and IL-8, exacerbating both periodontal and systemic inflammation, thus contributing to bone and tissue destruction similar to that seen in RA.
Changes in Oral Microbiota Composition
Studies comparing the subgingival microbiota of RA patients and healthy individuals have identified several microbial shifts. In RA patients, bacteria such as Prevotella, Leptotrichia, and Lactobacillus salivarius were more prevalent, while Haemophilus species decreased. These changes may reflect an altered oral microbial ecosystem that plays a role in disease modulation.
Osteoarthritis and Systemic Inflammation
Indirect Influence of the Oral Microbiome
Unlike RA, osteoarthritis is traditionally seen as a degenerative joint disease primarily driven by mechanical stress and aging. However, recent evidence suggests that systemic inflammation, potentially triggered by oral microbiota - may also play a role.
Oral pathogens and their byproducts, such as lipopolysaccharides (LPS), can enter the bloodstream through everyday activities like brushing or chewing, contributing to low-grade systemic inflammation that may influence OA progression.
Microbial Contributions to OA
Although the link between dental pathogens and OA is less direct, researchers have found differences in oral microbial composition among OA patients compared to healthy controls.
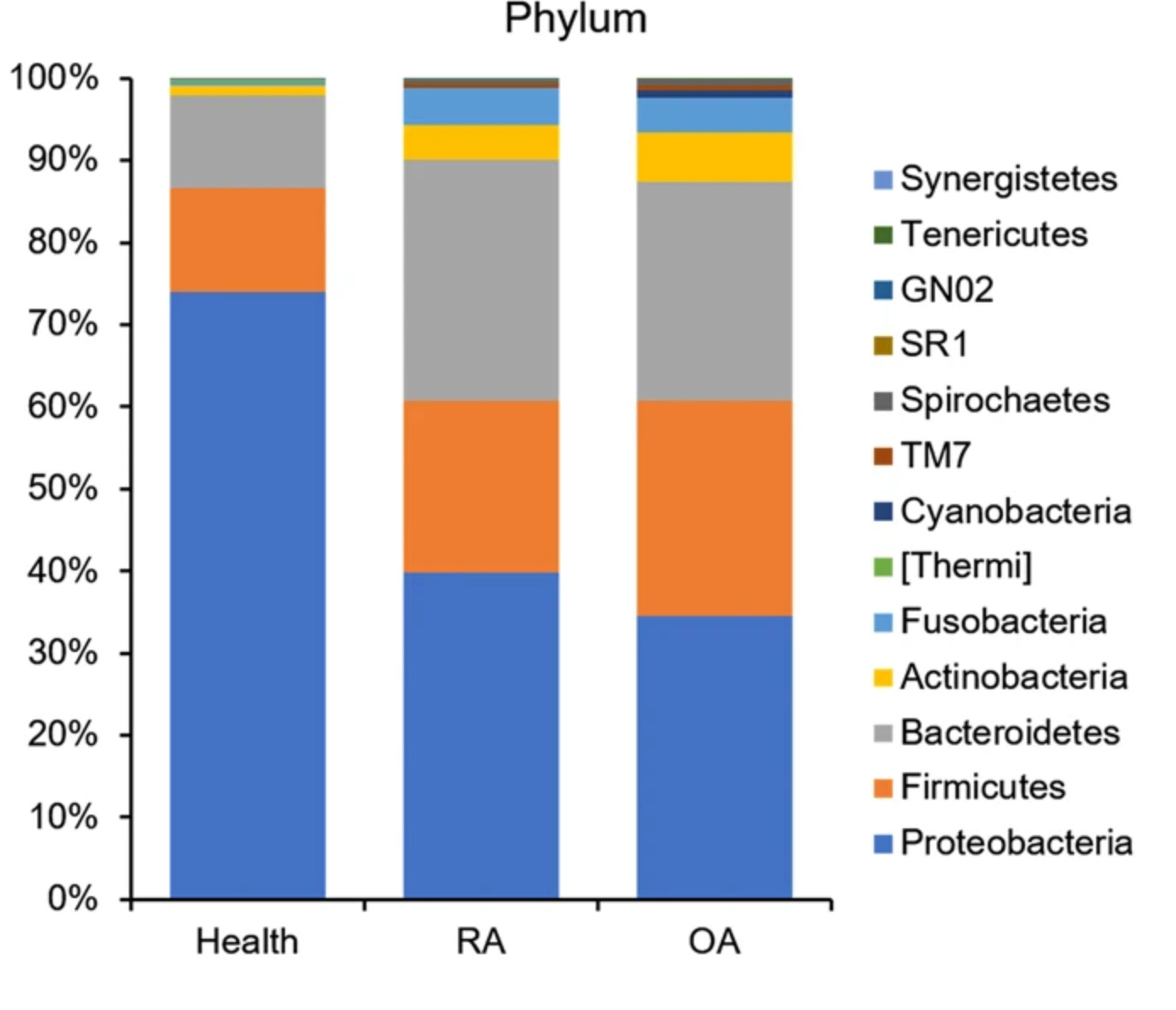
For example, the abundance of Firmicutes is higher in OA patients, whereas Proteobacteria are more prevalent in healthy individuals. This altered microbiota may contribute to systemic inflammatory responses that affect joint health.
Comparative Microbiota in RA, OA, and Healthy Individuals
In a large-scale study comparing the oral microbiota of 110 RA patients, 67 OA patients, and 155 healthy individuals, researchers noted distinct differences in microbial diversity and abundance:
RA-associated bacteria: Neisseria, Haemophilus, Veillonella, Prevotella, Actinobacillus, Fusobacterium, and Aggregatibacter.
OA-associated bacteria: Rothia, Ruminococcus, Streptococcus, Actinomyces, Lautropia, Granulicatella, and Oribacterium.
Interestingly, both RA and OA groups showed a higher diversity of oral bacteria compared to healthy controls, with an increase in potential opportunistic pathogens, most of which were Gram-negative anaerobes. This microbial shift supports the hypothesis that oral dysbiosis could influence the development or progression of arthritis.
Mechanisms of Microbial Translocation and Joint Inflammation
Oral bacteria have the ability to enter the bloodstream, especially in individuals with periodontal disease. Once in circulation, these microbes or their components, such as LPS, can localize in joints and activate immune responses.
LPS has been shown to:
- Correlate with joint inflammation and cartilage degradation.
- Upregulate pro-inflammatory cytokines involved in both RA and OA.
- Potentiate collagen-induced arthritis (CIA) in animal models.
- Promote biofilm formation, contributing to chronic infection and inflammation.
These mechanisms suggest a plausible route by which oral microbiota may influence bone health and contribute to the pathogenesis of both RA and OA.
Conclusion
While rheumatoid arthritis and osteoarthritis are distinct in origin and progression, both conditions may be modulated by oral health, particularly through interactions with the oral microbiome.
RA shows a clearer link to specific periodontal pathogens, notably Porphyromonas gingivalis, while OA may be indirectly influenced via systemic inflammation triggered by microbial translocation.
These findings highlight the importance of maintaining good oral hygiene and exploring the oral microbiome as a potential target for early diagnosis and intervention in arthritis. Continued research is necessary to further elucidate these connections and to develop microbiome-based diagnostic and therapeutic tools.
Other related posts:
5 Simple Ways to Manage Rheumatoid Arthritis Naturally - Part III
5 Simple Ways to Manage Rheumatoid Arthritis Naturally - Part II
5 Simple Ways to Manage Rheumatoid Arthritis Naturally - Part I
Osteoporosis Alert: The Hidden Danger of This Widely Used Drug
Osteoporosis? 4 Simple Solutions for Better Bone Health
Warning: This Supplement Increase Your Risk Of Heart Attack? Part I
Warning: This Supplement Increase Your Risk Of Heart Attack? Part II
🚨Join the 21-Day Metabolic & Insulin Reset Challenge - Week 1
🔥Fat Burning, Reboot Your Metabolism, Improve Insulin Resistance, Reclaim Your Energy.
✅ What Happens When You join the 21-Day Metabolic & Insulin Reset Challenge
✔ Burn fat more efficiently - even at rest
✔ Eliminate energy crashes or sugar cravings, improve gut health
✔ Support healthy weight loss without extreme dieting
✔ Improve insulin sensitivity and reduce the risk of type 2 diabetes
✔ Enjoy balanced, stable energy throughout your day
But….as a free subscriber, you’re missing out a lot!
When you upgrade your subscription now, you'll get access to
✅ 48-Hour Weight Loss Plan + Weekly Post to Beat Chronic Health Issues and Reclaim Your Health!
✅ Join the ONLY Monthly Health Challenge - Designed to Inspire Action and Deliver Results. This Isn’t Just Another Challenge 💥 This is a LIFESTYLE SHIFT that empowers you to take action, stay consistent, and achieve the health you’ve always wanted. 🌱
✅ Live or recorded Workshops, Webinars, or Podcasts with uncensored, unfiltered & no-nonsense perspectives on health. Deep dive on Immune System Reset, Gut Reset, and Brain Reset to reclaim your health.
✅ A 20-min Chat with me, followed by a personalized action plan sent straight to your inbox.
Join The VIP Inner Circle
🌟 48-Hour Weight Loss Plan+ Weekly Tips to Beat Chronic Health Issues and Reclaim Your Health! 🌟
✅ Join the ONLY Monthly Health Challenge - Designed to Inspire Action and Deliver Results -Immune System Rest, Gut Reset, and Brain Reset.
✅ Live or recorded Workshops, Webinars, and Podcasts with uncensored, no-nonsense perspectives on chronic health issues.
✅ A 20-min Chat with me, followed by a personalized action plan sent straight to your inbox.
✅ Exclusive Access to The Health Accelerator: A 60-minute 1:1 private coaching call twice a year with me (value $997) + Inner Circle access.
Remember knowledge is power and the more you know, the better decisions you can make for yourself and your loved ones.
If you like what you read, share it with your friends and earn subscription rewards when they subscribe.
If you find this information helpful, please share with your friends and family who may benefit from this information.
Would like to hear your thoughts about this topic:
References:
Kelsey JL, Lamster IB. Influence of musculoskeletal conditions on oral health among older adults. Am J Public Health. 2008 Jul;98(7):1177-83.
Moutsopoulos NM, Madianos PN. Low-grade inflammation in chronic infectious diseases: paradigm of periodontal infections. Ann N Y Acad Sci. 2006;1088:251-64. d
Lee YH, Hong SJ, Lee GJ, Shin SI, Hong JY, Chung SW, Lee YA. Investigation of periodontitis, halitosis, xerostomia, and serological characteristics of patients with osteoarthritis and rheumatoid arthritis and identification of new biomarkers. Sci Rep. 2024 Feb 21;14(1):4316.
Chen B, Zhao Y, Li S, Yang L, Wang H, Wang T, Bin Shi, Gai Z, Heng X, Zhang C, Yang J, Zhang L. Variations in oral microbiome profiles in rheumatoid arthritis and osteoarthritis with potential biomarkers for arthritis screening. Sci Rep. 2018 Nov 20;8(1):17126.
Rutger Persson G. Rheumatoid arthritis and periodontitis - inflammatory and infectious connections. Review of the literature. J Oral Microbiol. 2012;4.
Bingham CO 3rd, Moni M. Periodontal disease and rheumatoid arthritis: the evidence accumulates for complex pathobiologic interactions. Curr Opin Rheumatol. 2013 May;25(3):345-53.
Scher JU, Ubeda C, Equinda M, Khanin R, Buischi Y, Viale A, Lipuma L, Attur M, Pillinger MH, Weissmann G, Littman DR, Pamer EG, Bretz WA, Abramson SB. Periodontal disease and the oral microbiota in new-onset rheumatoid arthritis. Arthritis Rheum. 2012;64(10):3083-94.
These statements have not been evaluated by the Food and Drug Administration (FDA). These products or statements are not meant to diagnose‚ treat or cure any disease or medical condition. Please consult your doctor before starting any lifestyle changes, exercise or nutritional supplement program or before using these or any products especially during pregnancy or if you have a serious medical condition.